Menopause: An In-Depth Look At Women’s Change Of Life and Its Effect On Migraines
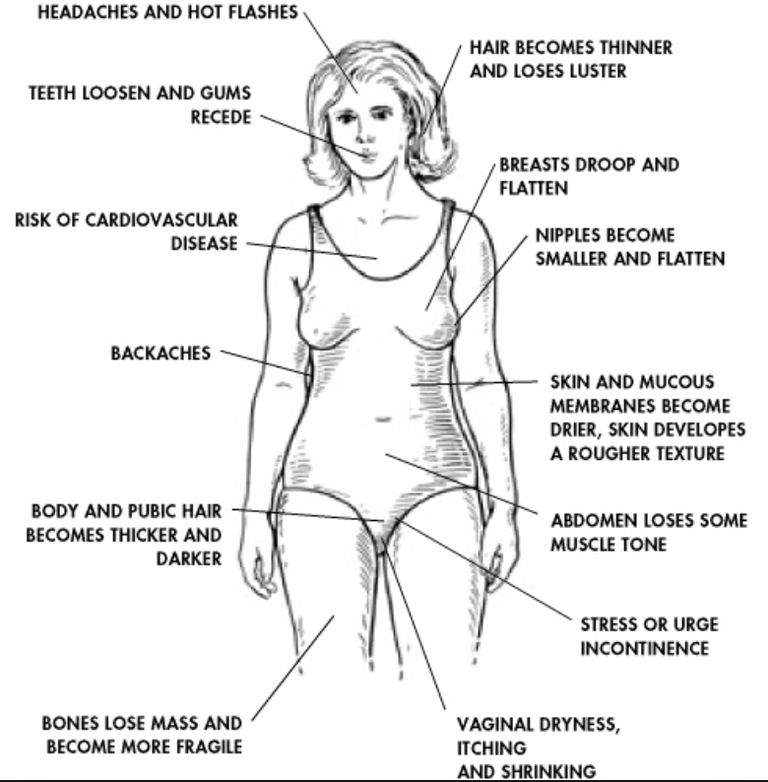
Medical professionals see menopause as being a woman’s final natural period. However, most people associate menopause with irregular periods and hot flashes – symptoms that are caused by aging ovaries and can begin 10 years or so before the woman actually has her last menstrual period. 90 percent of women experience headaches.

What Happens With Approaching Menopause?
Women who are about to go through the menopause face may endure worsening headaches and migraines on a more regular basis. They may find that the timing of these headaches is close to the time of their periods.
In the early menopause phases, periods come more often and are erratic, which can lead to more migraines. As the menopause comes to an end, the periods come less and less and as do the migraines. Women see the link between hormonal triggers and migraines, which is why they’re happy to see the end of the menopause stage. It can take up to three years before the last period and the hormones to settle down.
Non-hormonal triggers can be persistent even after the menopause phase.
What Happens In Menopause That Worsens The Migraines
The fluctuation in estrogen is the primary reason for a migraine to get worse. This is the hormone responsible for migraines worsening at puberty, which can take several years for the hormones to settle down. The majority of women – from the late teens to their mid-30s – experience a normal pattern of menstrual cycle hormones.
The natural decline in estrogen for some reason comes around the time of their menstruation. Some women may experience painful periods that are tied to migraines. Starting in their early 40s, the cycle varies because of the fluxes of estrogen levels. Periods may become more painful and bleeding may become heavier. These symptoms could cause migraines to worsen.
As the periods begin to slow down, so do the migraines. It’s why many people notice a drop in their migraines when they’ve gone through menopause.
Will HRT Alleviate Migraines?
While HRT isn’t used primarily for migraine treatments, many women have noticed that HRT can be effective in easing menopause symptoms such as night sweats, hot flashes and migraines. It’s important to understand that some versions of HRT can cause fluctuations in hormones that can lead to migraines – usually caused by HRT tablets.
Women who suffer from migraines are advised to use estrogen gel or patches to maintain their levels. The lowest estrogen dose, such as 25mcg of estrogen patches or 1 pump of gel, can help control the night sweats and hot flashes. This should be done for six weeks to see how the symptoms do. If they still persist, the dosages can be increased.
Special Note: It can be three months before the full effect of the HRT is felt, which is why women are advised not to increase the dosage too fast. While some women will need higher doses, they can be dropped once the symptoms ease.
Any woman who has not had a hysterectomy may need to use progestogens to protect the uterus lining from thickening due to estrogen. If not kept an eye on, it can become cancerous. Women who suffer from migraines and use progestogens can do so with estrogen patches or with the Mirena intrauterine system.
Should Women Consider Using Both the Mirena Coil and HRT?
The Mirena coil was designed to prevent pregnancy. However, it’s also now being used to control heavy, painful bleeding during menstruation. How so? It works right on the womb, which means the hormone stays in that general vicinity. There are very few side effects.
A woman with the Mirena coil can adjust their estrogen dose when necessary. They may discover that their periods stop entirely while using the coil. If their periods were the source of their migraines, the migraines are likely to subside as well.
When Is The Right Time To Quit Using Migraine Prevention Treatments After Menopause?
Doctors advise women to continue their migraine prevention treatments six months after menopause. After that, the dosage needs to be lowered over a period of three months. If the migraines come back, the dosage can increase to control the attacks for several more weeks before attempting to reduce the dosage.
This slow reduction will allow you to find the best dosage to handle the migraines and how long the treatment will be necessary.
Why Are Migraines Persistent Even After Menopause?
You may no longer experience periods, but it can take several years before the hormones stop fluctuating widely. While it’s just a couple of years, some women feel like it’s a lifetime. They may experience migraines and hot flash for many years after going through menopause.
While hormonal triggers have calmed down, it’s the non-hormonal problems that rear their ugly heads and increase in the post-menopause stage. Women may suffer from chronic conditions that worsen migraines. However, with healthy habits – regular exercise, eating healthy and a good sleep – these migraines will eventually subside.
Do Hysterectomies Worsen Migraine Symptoms?
Research has suggested that a hysterectomy can make migraines worse. The brain controls the menstrual cycle, as it tells the ovaries to fuel the production of progesterone and estrogen. These hormones will cause the womb lining to thicken, readying it for a possible pregnancy. If this doesn’t happen, the womb lining sheds and lead to menstruation.
When these are gone, the cycle is interrupted, and the brain hormones are unprepared for the early onset of menopause. This causes migraines to get worse, but eventually subside within two years’ time. With estrogen replacement therapy, the symptoms of early menopause will be easier to contend with. Even when the ovaries are still there after a hysterectomy, the natural cycle is still disturbed, and extra estrogen may be necessary.
Why Vaginal Estrogen Worsens Migraines
While vaginal estrogen is great in controlling the local symptoms of vaginal dryness and pain, it, unfortunately, causes migraines because of the sudden rise and drop in estrogen levels. This is especially hard for women who are susceptible to migraines. With a steady amount of estrogen in the body, the chances for migraines become less.
If you decide to use vaginal estrogen, it’s important to remember that migraines are possible with the treatment. If migraines do not ease after some time, you may need another treatment. If the key problem was vaginal dryness, you may need a lubricating gel, which contains no hormones that could lead to migraines.
